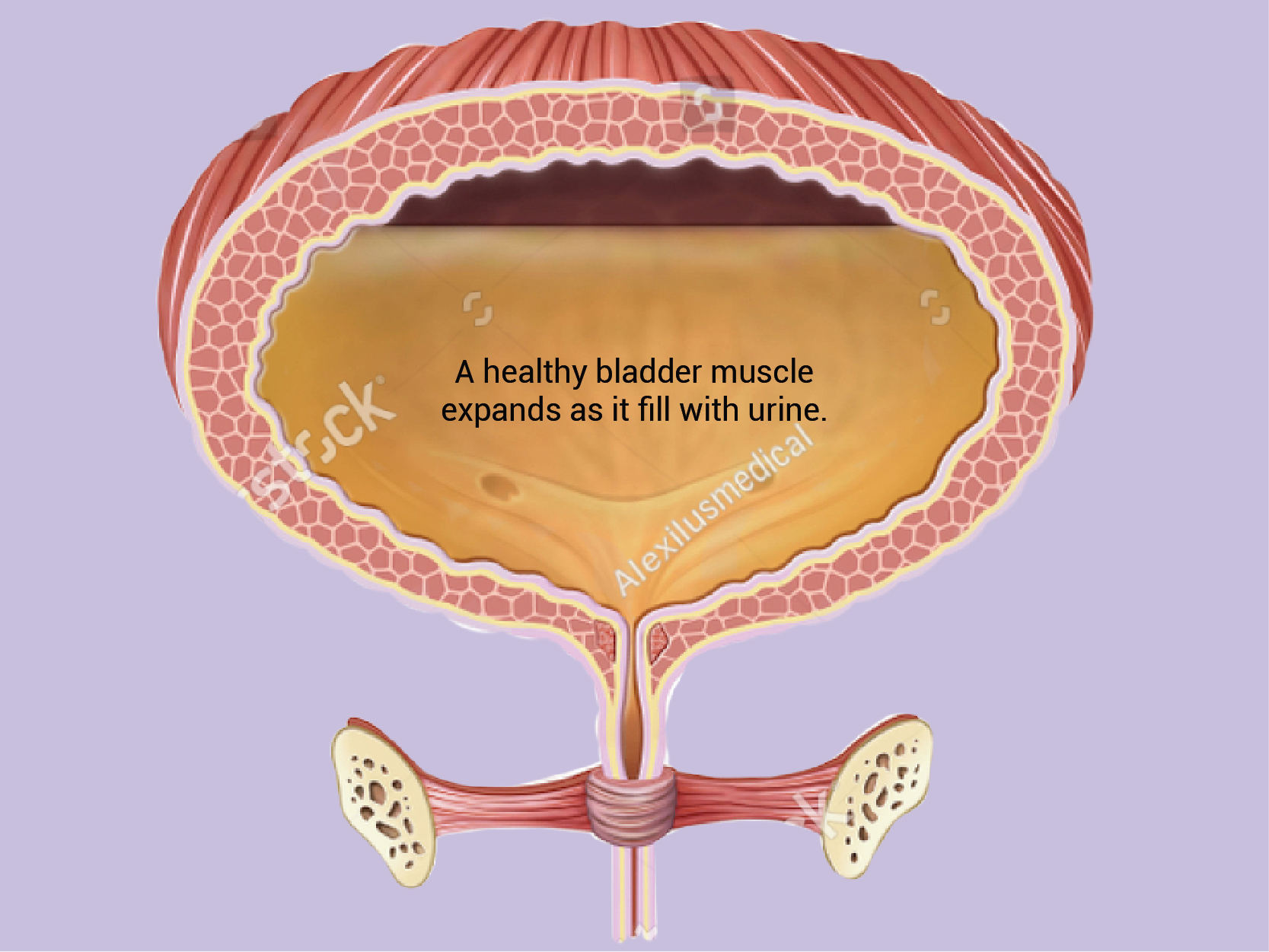
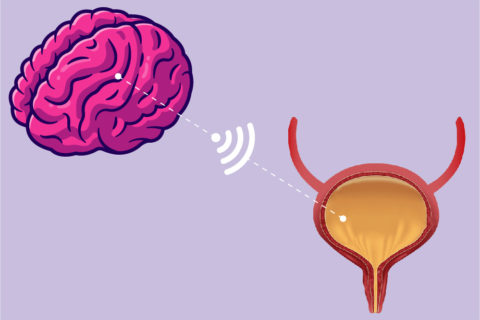
About overactive Bladder (OAB)
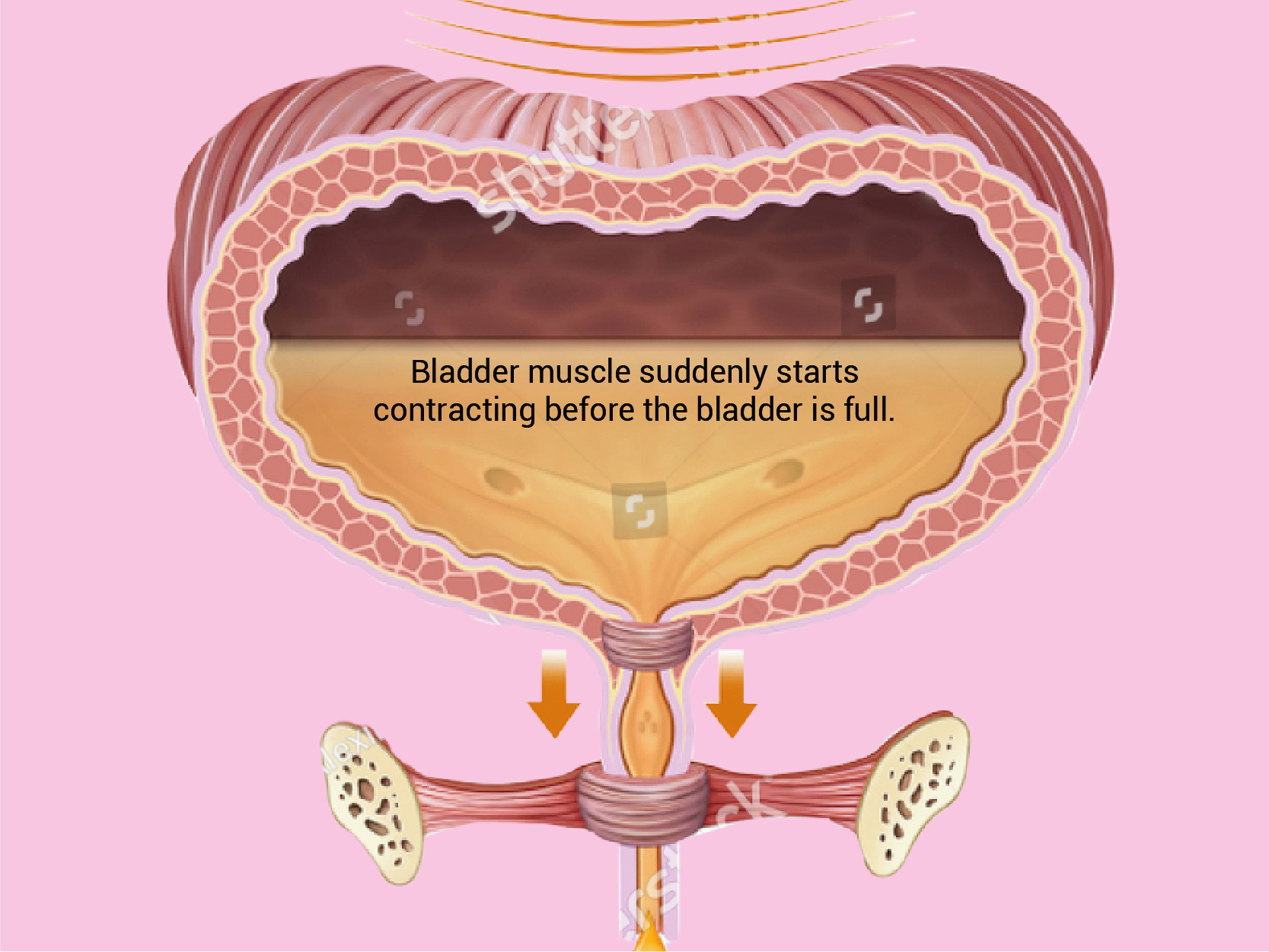
If you think you need to go to the washroom many times during the day, you have to wake up from sleep to go to the washroom more than once a night or your urine leaks when you feel the sudden urge to go
“It could be overactive bladder (OAB)!”